Health
Yobe, Others to Deliver Malaria Prophylaxis to 200,000 Children
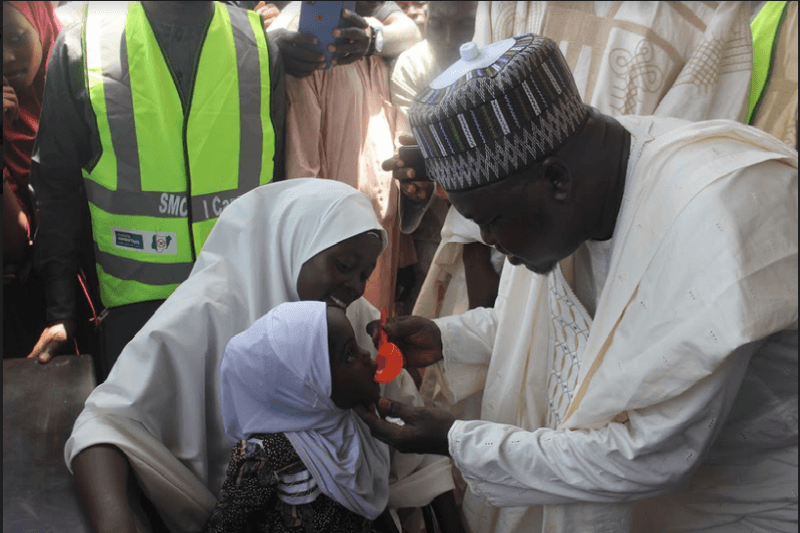
The government of Yobe State, through its Ministry of Health, has joined forces with the World Health Organisation (WHO) and Malaria Consortium to deliver seasonal malaria prophylaxis to nearly 190,000 children aged 03 – 59 months across 60 wards of six local government areas of the state.
These local councils are Yusufari, Tarmuwa, Bade, Machina, Nguru and Karasuwa. They reported highest malaria cases in 2018 in the state.
Yobe is one of three states mostly affected by the current humanitarian emergencies in north-east Nigeria. More than two-thirds of health facilities in the state are partially or not functioning leading to weakened healthcare service delivery, according to WHO health resources availability mapping system (HeRAMS) and malaria burden in 2018 was 70% among vulnerable populations that include children under five and pregnant women.
Overall, malaria accounts for more than half of all deaths recorded in North East Nigeria compared to other causes including cholera, measles and hepatitis E.
The seasonal malaria chemoprevention campaign being currently implemented at this auspicious time aims at maintaining an adequate level of antimalarial medicine concentration in targeted children in order to kill any malaria parasites during this period of high malaria transmission.
The Officer-in-Charge (OiC) of WHO Nigeria, Dr Clement Peter reiterated that WHO’s recommendation for seasonal malaria chemoprevention (SMC) campaign across the Sahel sub-region of Africa has proven to be an effective and evidence based intervention against malaria.
“Effective administration of SMC for up to four cycles during the peak of malaria transmission season among children aged 03–59 months could reduce malaria morbidity and mortality significantly,” said Dr Peter.
Representing the National Coordinator of the National Malaria Elimination Programme at the flag-off ceremony of the first SMC campaign in Gashua, Bade LGA, the Malaria Programme officer, Salisu Abdullahi Bogdoiri emphasized the importance of the exercise.
“With the seasonal malaria chemoprevention campaign coming barely one month after the mass distribution of long lasting insecticide nets, we expect that cases of malaria morbidity and mortality among children in Yobe state will decline.”
As of 2018, an estimated 198 million Nigerians were at risk of malaria, 57.3 million malaria cases were estimated to have occurred along with 81,640 deaths. This translated to 25 percent of global malaria cases being found in Nigeria and the country accounting for 19 percent of global deaths.
Although life-threatening, malaria is preventable and curable. With increased collaborative efforts to prevent the disease, the malaria burden can drastically be reduced and eventually eliminated in line with one of SDG 3’s target of having it eliminated by 2030.
Health
Union Disrupts NAFDAC Operations in Lagos Over Sachet Alcohol Ban

By Adedapo Adesanya
Members of the National Union of Food, Beverage and Tobacco Employees protested at the Lagos office of the National Agency for Food and Drug Administration and Control (NAFDAC), disrupting operations in reaction to the ban on sachet alcohol.
The protesting union members barricaded the agency’s premises in Isolo, meaning staff who arrived early to resume duty were forced to remain outside the complex.
Recall that NAFDAC has continued the ban on alcoholic beverages sold in sachets and PET bottles below 200 millilitres, despite calls from certain quarters, including the picketers.
The union is demanding the immediate unsealing of affected factories and production lines, warning that sustained enforcement of the policy could trigger significant economic consequences across the industry.
It is the second time this month that union members disrupted the Lagos NAFDAC office over what they described as the agency’s refusal to comply with an alleged federal government directive to suspend enforcement of the ban on the production and sale of alcoholic beverages in sachets.
The union claimed that directives had been issued by the Office of the Secretary to the Government of the Federation and the Office of the National Security Adviser, calling for the suspension of enforcement and the reopening of sealed production lines.
However, NAFDAC dismissed the claims, maintaining that it had not received any official instruction from the Federal Government to halt enforcement of the ban on sachet and PET-bottled alcohol.
Meanwhile, police officers were later seen at the NAFDAC Isolo premises, which dispersed the blockade to allow NAFDAC staff back into the premises.
Representatives of the Director-General of NAFDAC later engaged the protesting union in talks, but the meeting ended without resolution as demonstrators insisted their agitation would continue.
Union leaders presented their concerns during closed-door discussions with a director within the agency and the Special Assistant to the Director-General. However, no agreement was reached.
The protesters are urging NAFDAC to reconsider what they describe as the strict enforcement of the ban on sachet alcohol. Instead, they want the agency to focus on regulating access to such products, particularly by restricting sales to minors, while intensifying public enlightenment campaigns on responsible consumption.
Despite this, protesters say they will not stop until their demands are addressed.
Health
Modern Veterinary Clinics For Advanced Pet Care

As companion animals live longer and owners expect more from routine care, modern veterinary clinics have evolved into centers offering advanced diagnostics, specialty surgery, and integrative therapies. For busy professionals juggling work, travel, and online business demands, knowing which clinic delivers comprehensive care is essential. Frisco vet services illustrate how these modern practices combine cutting-edge technology, multidisciplinary expertise, and client-focused workflows. This article outlines the infrastructure, service offerings, and decision criteria that indicate a clinic capable of providing contemporary, evidence-based care while keeping visits efficient and stress-free for both pets and owners.
What Defines A Modern Veterinary Clinic
A modern veterinary clinic is defined less by a single piece of equipment and more by an integrated approach that combines up‑to‑date technology, specialized staff, and clinic design that prioritizes safety and comfort. These clinics treat animals with complex conditions, run efficient workflows, and communicate transparently with owners.
Key Infrastructure And Technology Investments
Contemporary clinics invest strategically in diagnostic and treatment modalities that materially change outcomes: digital radiography for rapid imaging, in‑house laboratories for same‑day blood work, ultrasound for real‑time organ assessment, and advanced surgical suites with anesthesia monitoring. Investment also includes infection‑control systems, reliable HVAC, and sterilization equipment. These capital decisions reduce turnaround time for diagnoses and support complex procedures that previously required referral.
Staffing, Specialization, And Continuing Education
Staffing reflects clinical ambition: veterinarians with specialty training (DACVS, DACVIM, DACVECC), certified veterinary technicians, and support staff trained in low‑stress handling. Modern clinics often host visiting specialists or maintain referral relationships with tertiary centers. Importantly, clinics that prioritize continuing education schedule regular training, subscribe to current literature, and engage in case reviews, actions that keep protocols current and improve outcomes.
Clinic Design For Safety, Flow, And Comfort
Design matters. Logical patient flow minimizes cross‑contamination and stress: separate entrances for healthy and sick patients, dedicated isolation wards, and distinct surgical zones. Comfortable client areas, clear signage, and private consultation rooms improve communication and compliance. For pets, non‑slip surfaces, quiet recovery areas, and pheromone‑friendly environments reduce anxiety, which in turn improves diagnostic accuracy and post‑procedure recovery.
Advanced Diagnostic Capabilities
Diagnostics are the backbone of modern pet care. Faster, more precise tests enable tailored treatment plans and earlier interventions.
Advanced Imaging: Digital X‑Ray, Ultrasound, CT, And MRI
Digital X‑ray provides high‑resolution images with immediate availability and easier sharing for remote consults. Ultrasound is indispensable for soft‑tissue evaluation and guided biopsies. CT and MRI, once exclusive to academic centers, are now present in many referral clinics, allowing detailed assessment of complex fractures, thoracic disease, neurologic conditions, and staging of cancer. Image quality and interpretation, often augmented by teleradiology, lead to more confident surgical planning and prognostication.
Laboratory, Point‑Of‑Care Testing, And Genomic Diagnostics
In‑house labs produce same‑day CBCs, chemistry panels, and cytology, accelerating decision‑making. Point‑of‑care tests for infectious agents, endocrine disorders, and clotting function add convenience without sacrificing reliability. Genomic diagnostics, from breed‑specific risk panels to tumor genomics, are increasingly accessible, enabling targeted therapies and risk stratification for hereditary conditions.
How Diagnostics Inform Preventive Care And Personalized Medicine
Diagnostics underpin preventive medicine: heartworm antigen tests, thyroid screening, and wellness blood panels reveal problems before clinical signs appear. Personalized medicine emerges when diagnostics inform individualized vaccination schedules, dietary plans, or monitoring frequency. The result: care that reduces emergency visits and improves long‑term quality of life.
State‑Of‑The‑Art Surgical And Interventional Services
Surgery in modern clinics spans routine spays and neuters to complex orthopedic reconstructions and image‑guided interventions.
Minimally Invasive, Laser, And Image‑Guided Procedures
Minimally invasive techniques, arthroscopy, laparoscopy, and endoscopy, reduce pain, shorten hospital stays, and speed return to function. Laser surgery provides precision and reduced bleeding for soft‑tissue procedures. Image‑guided interventions, such as CT‑guided biopsies or fluoroscopy for foreign body retrieval, allow targeted treatments that were once riskier or impossible.
Anesthesia, Pain Management, And Perioperative Safety
Anesthesia protocols are more nuanced today: individualized drug selection, multimodal analgesia, regional blocks, and continuous monitoring (ECG, capnography, pulse oximetry) improve safety. Preoperative assessment, including risk stratification and optimization of comorbidities, reduces complications. Recovery protocols emphasize early mobilization and aggressive pain control to prevent chronic pain syndromes.
Postoperative Rehabilitation And Recovery Protocols
Rehabilitation is an expected component of surgical care. Physical therapy, hydrotherapy, and tailored exercise plans reduce muscle atrophy and improve joint function. Clinics often provide home‑care instructions and scheduled reassessments to track progress and adjust protocols. These programs turn good surgical outcomes into durable functional gains.
Petfolk Veterinary & Urgent Care – Frisco
Advanced Therapeutics And Specialty Treatments
Beyond diagnostics and surgery, modern clinics deliver advanced therapeutics that extend and improve life quality.
Regenerative Medicine: Stem Cells And PRP
Regenerative modalities like mesenchymal stem cell therapy and platelet‑rich plasma (PRP) injections aim to stimulate healing in tendon, ligament, and osteoarthritic conditions. While still an evolving field, controlled studies and clinical experience show promising functional improvements for select patients. Clinics offering these therapies combine careful case selection with measurable outcome tracking.
Oncology, Neurology, Cardiology, And Other Specialties
Specialty services allow complex, multidisciplinary care. Veterinary oncologists provide staging, chemotherapy, and radiation planning: neurologists manage seizure disorders and spinal disease: cardiologists use echocardiography and interventional procedures for congenital heart defects. Integration with imaging and lab diagnostics enables cohesive care pathways that mirror human tertiary centers.
Integrative Therapies: Physical Rehab, Acupuncture, And Nutrition
Integrative care recognizes the value of adjunctive treatments. Acupuncture and targeted nutrition plans complement medical therapy for chronic pain and mobility issues. Nutritional counseling, including therapeutic diets for renal, cardiac, or dermatologic disease, is standard in clinics focused on long‑term outcomes.
Improving Pet And Client Experience With Technology
Technology enhances both clinical care and client experience, especially for owners who need efficient, transparent services.
Telemedicine, Remote Monitoring, And Virtual Follow‑Ups
Telemedicine extends access for triage, follow‑ups, and behavioral consultations. Remote monitoring devices, activity trackers, continuous glucose monitors, and wearable ECGs, provide objective data between visits. Virtual follow‑ups reduce travel burdens and let clinicians adjust care in real time, improving adherence and satisfaction.
Electronic Medical Records, Client Portals, And Scheduling Tools
Electronic medical records (EMRs) streamline documentation and support coordinated care. Client portals give owners access to vaccination histories, lab results, and discharge instructions. Integrated scheduling and automated reminders decrease no‑shows and improve preventive care compliance, a benefit both to clinics and busy clients.
Pain Management, Behavior‑Based Care, And Low‑Stress Handling
Client experience is inseparable from pet comfort. Modern clinics train staff in low‑stress handling techniques and behavior‑based protocols that reduce fear and aggression. Transparent pain‑management plans, clear cost estimates, and follow‑up communications foster trust and better outcomes.
How To Choose The Right Modern Clinic For Your Pet
Choosing a clinic requires practical criteria and an understanding of trade‑offs between convenience, specialization, and cost.
Questions To Ask: Credentials, Equipment, And Outcomes
Prospective clients should ask about specialist credentials, the availability of imaging and lab services, and the clinic’s approach to anesthesia and pain control. Request examples of similar cases and expected outcomes. A clinic that welcomes such questions is often more transparent and results‑oriented.
Cost, Insurance, And Referral Pathways
Advanced care carries higher costs. Discuss fee structures, payment options, and whether the clinic works with pet insurance. Understand referral pathways: does the clinic refer to or host board‑certified specialists? Clear referral and co‑management policies indicate maturity and a networked approach to care.
Evaluating Reviews, Accreditation, And Collaboration With Primary Vets
Look for consistent reviews that mention communication, follow‑up, and outcomes rather than isolated flashy cases. Accreditation (AAHA in the U.S.) or affiliation with universities can signal adherence to higher standards. Finally, the best specialty clinics collaborate with primary care veterinarians, ensuring continuity rather than competition.
Conclusion
Modern veterinary clinics for advanced pet care combine technology, specialization, and thoughtful design to deliver better diagnostic accuracy, safer surgeries, and more personalized therapies. Pet owners benefit when clinics pair capabilities with clear communication, transparent costs, and collaborative care models. For professionals, including small business owners and busy entrepreneurs who value efficient, outcome‑driven services, selecting a clinic that integrates advanced diagnostics, robust perioperative care, and client‑centric technology yields the best chance for sustained pet health. As veterinary medicine continues to mirror human healthcare in capability and complexity, informed choices and trusted partnerships between owners and clinics will determine the real value of those advances.
Health
Oyo Seals Ar-Rahmon Khabul Herbal Over Health Concerns

By Modupe Gbadeyanka
An Ibadan-based herbal company, Ar-Rahmon Khabul Herbal Nigeria Limited, has been sealed by the Oyo State Rule of Law Enforcement Authority (OYRLEA).
The state government, in a statement signed on Friday by the Commissioner for Information, Mr Dotun Oyelade, revealed that the herbal firm was shut down due to environmental violations and public health concerns.
The leader of OYRLEA, Mrs Aderonke Aderemi, explained that the action was taken after multiple petitions from residents alleging persistent offensive odour and health challenges linked to the company’s operations.
She noted that the state government swung into action “to protect public health, preserve environmental standards, and enforce regulatory compliance across the state.”
It was gathered that investigations identified tobacco leaf as a major component in its production process, generating a strong, putrid odour deemed hazardous to residents and capable of posing serious health risks to the surrounding community.
“Joint inspections by officials revealed that the company operates a herbal production facility within a densely populated residential area, in clear violation of environmental and public health standards,” the statement said, adding that further findings from the inspection include the emission of harmful and toxic gaseous substances into the atmosphere, the discharge of wastewater into a nearby community water body, the installation of a chimney deemed too short and directly facing residential buildings, and the accumulation of solid waste within the premises despite claims of engaging a waste contractor, among others.
Prior to the enforcement action, the agency had issued an abatement notice directing the company to cease operations and relocate within 21 days in accordance with the Oyo State Environmental, Sanitation and Waste Control Regulations.
OYRLEA, along with the agencies that carried out the enforcement, reiterates that air pollution, hazardous waste discharge, and improper waste management are violations of environmental laws.
Mrs Aderemi reaffirmed OYRLEA’s commitment to sustained monitoring and enforcement to ensure a safe and healthy environment for all residents.
-

 Feature/OPED6 years ago
Feature/OPED6 years agoDavos was Different this year
-
Travel/Tourism10 years ago
Lagos Seals Western Lodge Hotel In Ikorodu
-

 Showbiz3 years ago
Showbiz3 years agoEstranged Lover Releases Videos of Empress Njamah Bathing
-

 Banking8 years ago
Banking8 years agoSort Codes of GTBank Branches in Nigeria
-

 Economy3 years ago
Economy3 years agoSubsidy Removal: CNG at N130 Per Litre Cheaper Than Petrol—IPMAN
-

 Banking3 years ago
Banking3 years agoSort Codes of UBA Branches in Nigeria
-

 Banking3 years ago
Banking3 years agoFirst Bank Announces Planned Downtime
-

 Sports3 years ago
Sports3 years agoHighest Paid Nigerian Footballer – How Much Do Nigerian Footballers Earn