Health
Five Lessons Learned During Latest Ebola Outbreak in DRC

By MSF
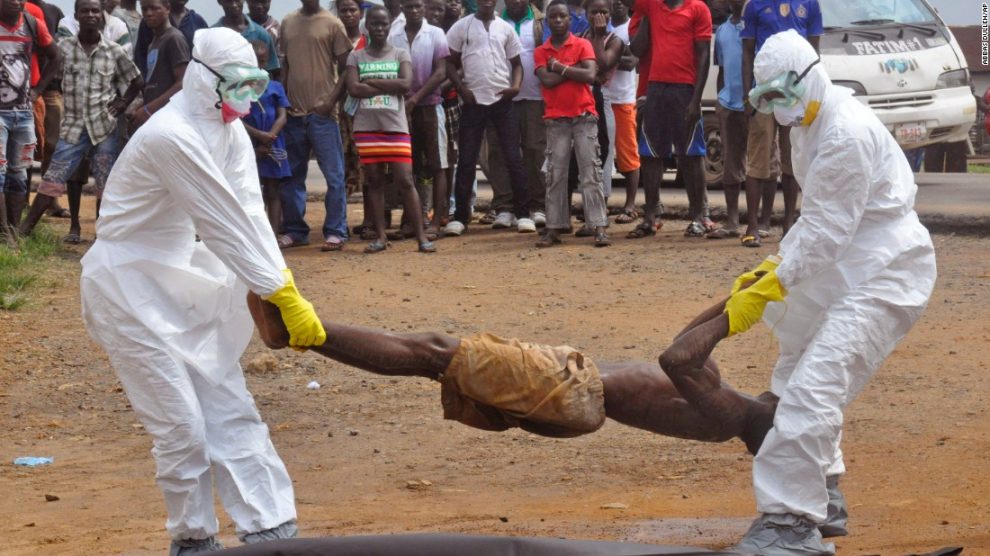
Four people died in the most recent Ebola outbreak that occurred in a remote, forested area of the Democratic Republic of Congo (DRC).
This small outbreak (five laboratory-confirmed and three probable cases) was quickly curtailed. The international humanitarian organisation Doctors Without Borders (MSF) shares lessons learned from this first occurrence of the deadly virus since the end of the large-scale Ebola outbreak that devastated West Africa in 2014-2015.
Train frontline health teams
The scale of this outbreak was minimised, thanks in no small part to a nurse named Dieumerci. With a name that literally translates to ‘Thank God’ in French, Dieumerci works at a Ministry of Health centre in northeast DRC, where the first Ebola cases started emerging.
He detected the risk of Ebola in a seriously ill man at the hospital, and rang the alarm. This man turned out to be the second confirmed case during the recent outbreak. Unlike in West Africa prior to the last major outbreak, Ebola is known in the DRC: the Ebola River, where the virus was first discovered, runs 100 kilometres away from where Dieumerci works.
That doesn’t mean that it is common disease in the area, but still, Dieumerci recognised the symptoms. His quick actions should not be taken for granted. Healthcare workers play a crucial role not only for patients, but also for general epidemiological surveillance. However, in many developing countries human resources within the health sector remain starkly inadequate.
On that fateful day where the Ebola patient came to the health centre, Dieumerci could have easily been on a sick leave, or visiting family somewhere else in the country. One cannot rely on a single individual to play the crucial role of on-the-ground surveillance.
What is needed are proper surveillance systems in resource-poor countries, which were clearly lacking in West Africa at the time of the epidemic. So all in all: thank you Dieumerci. We should all hope that during the next outbreak – be it Ebola or any other infectious disease – there will be another Dieumerci to ring the alarm bell for everyone’s sake.
Finally, a forgotten disease is taken seriously
The word “Ebola” doesn’t ring the same after 2014-2015’s devastating epidemic. At least 11,300 people were killed, and over 28,000 were infected. As a result, Dieumerci’s alarm bell sent shock waves across the world. Congolese authorities immediately activated their outbreak response team and had strong support from WHO and other organisations.
Henry Gray, MSF’s project coordinator during this recent outbreak, has worked on seven haemorrhagic fever interventions in DRC, Uganda and West Africa, to name a few. “The pressure we felt was very different from previous comparable outbreaks: it was clearly at the top of the agenda,” he says. “When it comes to Ebola, we have all learned that it’s better to be safe than sorry in order not to repeat the disaster of 2014-2015.
“However, it is sad to still see that other outbreaks in countries do not trigger the same mobilisation, even in regards to the main killer diseases like cholera or measles.
“Once the Ebola outbreak was over, we were able to re-assign some of the MSF staff towards a serious cholera outbreak on the other side of the country. Our teams went on to treat 1,100 cholera patients. “Considering the dire health needs in many parts of the country, additional support is always welcome”.
Old tricks are timeless – back to basics
The promise of new drugs or vaccines should not overshadow the necessity of putting in place the basic pillars of outbreak control.
It all starts with good surveillance, followed by the five pillars of outbreak control:
Safely isolating and treating the sick.
Actively looking for potential new cases and surveilling those who have been in contact with them.
Burying the dead safely.
Engaging and mobilising the affected communities.
Offering psychological support.
In West Africa, the havoc wrecked by Ebola on the entire health system created more indirect than direct victims of the virus: children became prone to infectious diseases because they weren’t vaccinated; Childbirth complications led to the deaths of mothers and/or children because there were no healthcare workers to care for them; untreated cases of malaria became fatal…
International health actors need to do more to support local health facilities that often have much smaller means and equipment: training staff, ensuring there is basic protection equipment available, and that their pharmacies are stocked with first aid supplies and basic medicines. Our experience in DRC has shown that training frontline workers, even when done ad-hoc, can bring sustained effects to improve their performance in surveillance.
Location, location, location
Like the majority of haemorrhagic fever outbreaks prior to West Africa, the recent one occurred in a very remote, forested area.
Here, the virus was already known to exist within an animal reservoir (assumed to be fruit bats) that is occasionally transmitted to apes, monkeys or men. Some people are very mobile in the region, but can only go as far and as fast as their available transportation; which is pretty much nothing beyond walking and the occasional motorbike.
Dieumerci’s village is 45 kilometres from Likati, the closest town. It is home to 18,000 people, with a majestic cathedral and large, but under equipped, hospital serving as remnants of a time when a railroad was still linking plantations across the country. Today that railroad has been eaten by the encroaching jungle. By contrast, in Guéckédou, Guinea – where the West Africa outbreak started – people can jump on a motorbike and be in the heart of the capital Conakry and its 2.5 million people within two days.
These contrasting examples show how isolation from major cities can keep the spread of deadly disease under control.
Medical innovations are not the magic bullet
At the time of the latest outbreak, MSF was willing to use Ebola treatments which were still in development. However this window closed as the outbreak stopped before the process to allow the use of the experimental treatments was complete. However, this event acted as a ‘booster’ – speeding up the process of preparing medical protocols so that new drugs (still in the experimental phase) can be used in ways that are as safe and ethical as possible.
The rVsV-ZEBOV vaccine (the most advanced investigational vaccine candidate for an Ebola outbreak today) is in development, and needs to be implemented through a study protocol. This, and a vaccine strategy – including informed consent under good clinical practice – were mandatory requirements needed from us to access them.
Soon enough, a study protocol was developed and approved by the MSF Ethics Review Board a few months ago. It was ready for implementation should an outbreak occur. Additionally, a dedicated MSF research team was ready to be deployed. Unfortunately, our negotiations at the DRC Ministry of Health level only took place when the outbreak had already been declared.
It took some time for us to explain what we were planning to do, and how this would differ from a vaccination campaign. But, we managed to obtain authorisation from all the regulatory bodies to start activities in case of a future outbreak.
It is likely that the next outbreak (and trust us, there will be a next outbreak) will happen in a similar setting. We can continue to learn how to best tackle it, and ensure that the West Africa Ebola outbreak remains an isolated tragedy.
Since 1990 MSF has responded to over a dozen outbreaks in sub-Saharan Africa. During the devastating Ebola outbreak that struck mainly Liberia, Guinea, and Sierra Leone in 2014-2015, MSF launched one of the largest emergency operations in its 44-year history.
MSF admitted 10,310 patients to its Ebola management centres of which 5,201 were confirmed Ebola cases, representing one-third of all WHO-confirmed cases. During the first five months of the epidemic, MSF handled more than 85 percent of all hospitalized cases in the affected countries.
At the peak of the epidemic, MSF employed nearly 4,300 staff—most of whom were from the affected countries—who ran Ebola management centres, conducted surveillance, contact tracing, and health promotion, and provided psychological support.
Health
Codix Bio Strengthens Nigeria’s Healthcare Manufacturing With New Sagamu Factory

By Aduragbemi Omiyale
A new rapid diagnostic test (RDT) production plant has been opened in Sagamu, Ogun State by Codix Bio Limited in a bid to strengthen healthcare manufacturing in Nigeria.
The Governor of Ogun State, Mr Dapo Abiodun, commended the company for choosing the state for the factory, which he described as a transformative leap to making the country a big force in the healthcare system.
“We are proud to commission Nigeria’s first large-scale rapid diagnostic test (RDT) production facility—Codix Bio Limited—right here in Ogun State.
“Located along the Sagamu Expressway, this state-of-the-art in-vitro diagnostics factory is only the second of its kind in Sub-Saharan Africa and will produce over 147 million test kits annual for diseases such as HIV, Malaria, and Hepatitis B and C.
“This milestone marks a transformative leap in our journey to strengthen Nigeria’s healthcare system through bold investment, local innovation, strategic partnerships, and local manufacturing,” he stated.
With this facility, Codix Bio is now the first African manufacturing partner selected by the World Health Organization (WHO), SD Biosensor, and the Medicines Patent Pool (MPP) under the WHO Health Technology Access Pool (HTAP) programme.
This landmark designation places Codix Bio at the forefront of regional production for RDTs in Africa—solidifying its role as a key partner in strengthening global health security.
The new plant positions the firm within the scope of WHO’s technical support system, allowing for technology transfer, regulatory assistance, and sustained global collaboration.
Through the sublicensing agreement with SD Biosensor and MPP, Codix Bio will receive proprietary rights, technical know-how, and materials to legally develop and produce rapid diagnostic test kits based on SD Biosensor’s cutting-edge platform.
This technology enables the production of multipurpose rapid diagnostics adaptable to both pandemic and inter-pandemic periods marking a transformative milestone in increasing equitable access to healthcare in low- and middle-income countries (LMICs).
With the commissioning of this facility, Codix Bio is scaling innovation and it has positioned Nigeria and the African continent for self-reliant, sustainable healthcare solutions.
“With over 90 per cent of diagnostic kits used in Africa currently imported, this facility will significantly reduce our reliance on external supply chains, conserve foreign exchange, and create high-value jobs.
“This factory will help to solidify Nigeria’s position as a health hub in the continent and globally. This is a leap forward for our national and continental health security,” he affirmed.
“With this facility, we are not only boosting local production but also saving foreign exchange, creating jobs, and reinforcing our public health response capacity.
“We call on other investors to come onboard by producing other medical consumables needed by the various medical diagnostic groups,” the Coordinating Minister of Health and Social Welfare, Professor Muhammad Ali Pate, said.
On his part, the WHO Representative in Nigeria, Dr Walter Kazadi Mulombo, hailed the facility as a “game-changer” in Africa’s efforts toward disease control, health security, and public health advancement, saying it will improve access to timely and accurate testing and reduce dependence on imported rapid test kits.
The chairman of Codix Pharma Group, Mr. Sammy Ogunjimi, said, “We are delighted to unveil our second manufacturing plant today. But beyond infrastructure, we know that human capital is equally vital.”
He reiterated Codix Pharma’s support for regional integration frameworks, including the Africa CDC, the African Continental Free Trade Area (AfCFTA), and the African Medicines Agency (AMA).
“Once a product is approved by NAFDAC, it should move freely across Africa. Regulatory harmonization is essential to unlocking the potential of intra-African health trade,” he said.
Health
Ondo Governor Tasks Mothers to Become Immunisation Advocates

By Dipo Olowookere
The Governor of Ondo State, Mr Lucky Aiyedatiwa, has urged mothers in the state to join the state government and others like the World Health Organisation (WHO) to promote vaccination.
Speaking during the 2025 African Vaccination Week at the Comprehensive Health Centre in Isolo, Akure on April 24, 2025, Mr Aiyedatiwa, represented by his Special Adviser on Health, Professor Michael Sinmidele Odimayo, charged mothers to become immunisation advocates.
“Inform those ignorant about vaccination and its importance. Vaccination is a human right,” the Governor said, highlighting the state’s health priorities, including free Hepatitis B treatment and the expansion of the health insurance scheme.
Delivering WHO’s goodwill message on behalf of the Country Representative, Dr Walter Kazadi Mulombo, Dr Adebayo said, “The African Vaccination Week is a reminder of WHO’s commitment to ensuring every child has access to life-saving vaccines.
“Immunisation is a human right, and this year’s theme is a powerful call to action. We appreciate all caregivers and partners championing this cause.”
Business Post gathered that about 70 children were immunised and administered doses of the Oral Polio Vaccine (OPV), Rota vaccine, and Vitamin A.
To encourage continued participation and advocacy, all 70 caregivers received diapers as incentives and were recognised as immunisation champions.
One of them, a 30-year-old Ajibola Ibukunoluwa, said vaccination is a must, stressing that, “Immunisation reduces mortality in children, and I’ll keep encouraging others to get their children vaccinated. The vaccination week has helped raise awareness among mothers.”
Another caregiver, Mrs Hassan Olayinka, whose 9-month-old baby received the measles, yellow fever, and meningitis vaccines at the event, expressed her gratitude to the government, WHO, and partners for making the vaccines accessible and available to children in the country.
“Immunisation is a very powerful tool. It prevents children from falling sick. I am happy with the services I received today and will advise mothers in my neighbourhood to take it seriously. I thank the State Government and partners like WHO for organising this,” she stated.
The immunisation programme was organised by the state government through the Ondo State Primary Health Care Development Agency (OSPHCDA), in collaboration with WHO, Clinton Health Access Initiatives (CHAI) and UNICEF to mark the 14th African Vaccination Week themed Immunisation for all is Humanly Possible.
Health
Stanbic IBTC Intensifies Fight Against Malaria, Impacts Over 5,000 Lives

By Modupe Gbadeyanka
Over 5,000 lives were impacted through the nationwide malaria initiative of Stanbic IBTC Holdings Plc across Enugu, Delta, and Kano States last month.
The company delivered free malaria testing and diagnosis; administration of treatment drugs to those who tested positive; awareness talks on malaria prevention and distribution of long-lasting insecticidal nets (LLINs) to residents of the communities visited by its team.
The programme was in commemoration of World Malaria Day 2025 themed Malaria Ends With us: Reinvest, Reimagine, Reignite, which was used to call for renewed commitment to malaria prevention and control efforts.
It was gathered that on April 25, Stanbic IBTC was at Nchatancha in Enugu East Local Government Area (LGA), and went to Okpanam in the Oshimili North LGA of Delta State on April 28, and climaxed the visit to Wudil Ward in Wudil LGA, Kano State on April 30.
“We are proud to support World Malaria Day 2025 and contribute to global efforts to control and eliminate malaria.
“Our partnership with stakeholders has helped raise awareness about the disease; promote prevention and control measures; and inspire action towards achieving a malaria-free world,” the acting chief executive of Stanbic IBTC Holdings, Mr Kunle Adedeji, stated.
The initiative comes at a critical time when sustainable investment in malaria prevention is needed to protect vulnerable populations.
According to the World Health Organization (WHO), there were an estimated 263 million malaria cases and 597,000 deaths worldwide in 2023 – representing about 11 million more cases compared to 2022.
Nigeria bears a disproportionate burden of the disease, accounting for 30.9 per cent of all malaria deaths in the WHO African Region. Children under five years old account for approximately 76 per cent of all malaria deaths in the region, making timely interventions crucial for survival.
Through its comprehensive programme, Stanbic IBTC continues its long-standing commitment to promoting health, well-being, and sustainable development in the communities it serves. By focusing on grassroots engagement, the financial institution ensures that life-saving information and resources reach those most at risk.
The campaign represents a model for effective corporate intervention in public health challenges. By supporting prevention, early diagnosis, and effective treatment strategies, this initiative helps save lives and strengthens community resilience against this preventable and treatable disease.
Stanbic IBTC’s malaria intervention aligns with global efforts that have averted an estimated 2.2 billion cases of malaria and 12.7 million deaths since 2000, according to the WHO.
-

 Feature/OPED5 years ago
Feature/OPED5 years agoDavos was Different this year
-
Travel/Tourism9 years ago
Lagos Seals Western Lodge Hotel In Ikorodu
-

 Showbiz2 years ago
Showbiz2 years agoEstranged Lover Releases Videos of Empress Njamah Bathing
-

 Banking7 years ago
Banking7 years agoSort Codes of GTBank Branches in Nigeria
-

 Economy2 years ago
Economy2 years agoSubsidy Removal: CNG at N130 Per Litre Cheaper Than Petrol—IPMAN
-

 Banking2 years ago
Banking2 years agoFirst Bank Announces Planned Downtime
-

 Sports2 years ago
Sports2 years agoHighest Paid Nigerian Footballer – How Much Do Nigerian Footballers Earn
-

 Technology4 years ago
Technology4 years agoHow To Link Your MTN, Airtel, Glo, 9mobile Lines to NIN