Health
Assault: The Albatross of LASUTH Healthcare Workers
By Olutayo Irantiola
The spate of physical violence in our society has increased tremendously, daily; the media is inundated with the news of all forms of assaults. It seems as if people have not taken lessons from all this reportage as it keeps rising astronomically. Unfortunately, this ugly trend has not spared healthcare workers and this is a dangerous position that must be discouraged.
The World Health Organization (WHO) defines workplace violence as, “Incidents where staff are abused, threatened, or assaulted in circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being, or health.”
WHO considers both physical and psychological harm, including attacks, verbal abuse, bullying, and both sexual and racial harassment, to be workplace violence.
In a study conducted by the New England Journal of Medicine, there are 4 types of violence that can occur in the workplace. The first type is by perpetrators who have no association with the workplace or employee.
In the second type, the assailant is a customer or a patient of the workplace or employee. The second type of violence, usually committed by the patient, their families, or their friends, is most prevalent against healthcare workers.
A third type is when the attacker is a current or former employee of the workplace. The fourth type occurs when the perpetrator has a personal relationship with the employee but not with the workplace.
Also, in an article published by BMC Health Services Research titled Manifestations of verbal and physical violence towards doctors: a comparison between hospital and community doctors by Tamar Nevo et al, doctors often are a target for workplace violence.
About a quarter of emergency room doctors reported that they were the victims of physical abuse over the previous year. In a study conducted at Michigan University, 89% of the violent incidents were by patients, 9% by family members, and 2% by friends of the patient.
The primary reasons for violence directed at the medical staff are long waiting times, dissatisfaction with treatment, a hurtful comment by a staff member, or the influence of drugs and alcohol on the attacker.
According to the US Department of Labour, 12% of the injuries sustained by registered nurses are from violent acts. These injuries can be deadly.
Last year in Nigeria, the former National President of Nigerian Association of Resident Doctors (NARD), Dr Aliyu Sokomba, Secretary-General, Dr Bilqis Muhammed, and Publicity and Social Secretary, Dr Egbogu Stanley, the association condemned the recent attack on members who were performing their legitimate duties in Maitama District Hospital, Abuja and Nnamdi Azikiwe University Teaching Hospital, Nnewi.
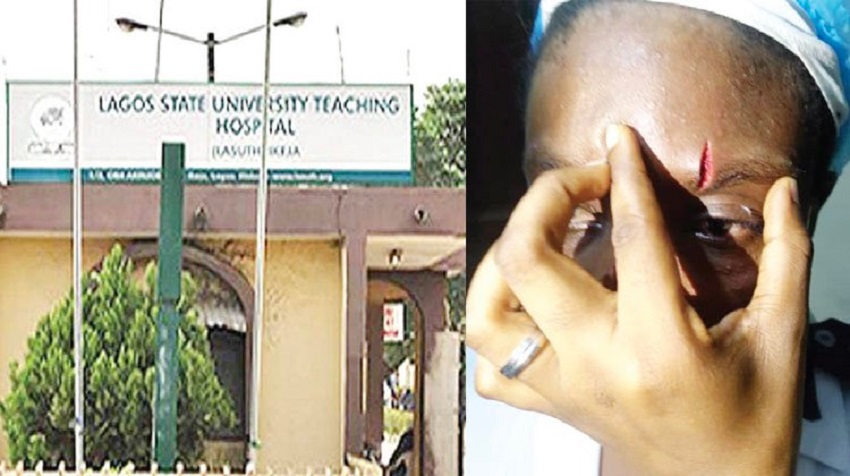
The recent happening at the Lagos State University Teaching Hospital (LASUTH) wherein the relative of a patient, who was presented with a gunshot injury, assaulted the staff has brought the discourse to the fore again.
In the process of trying to resuscitate the patient, the relative attacked 3 nurses and a doctor in the line of work. In fact, one of the nurses had a deep cut on the head, while one was almost stripped naked. However, the security personnel of the hospital later got him apprehended and arrested.
With the significant rise in the population of Lagos, both in numbers and in age, the waiting time to see a doctor gets longer in both the emergency room and the wards. These frequent acts of violence against employees can have on their morale over time.
“Emergency care is one of the specialties that do have a high burnout rate. How many other places do you go to work, and it’s commonplace and almost accepted that people are going to swear and scream at you? Eighty per cent of the emergency physicians say that patients threaten them or threaten to return to the emergency department to harm them. The cumulative effect of both kinds of violence does wear and it creates burnout. I think it’s contributing to nurses leaving the profession.”
Although the hospital has put up “zero tolerance” signs, patients and their relatives do not adhere to this instruction. With the various ways of escalating the pain of patients and their relatives to the hospital management, people still find it easier to be violent rather than engage with the management team. Every day across the country, people are verbally and physically abusing staff.
The apprehended relative of the patient has been taken to court and the law would take its due course. All hands are on deck waiting for the verdict. It is wise to state that everyone needs to be calm even in the face of utmost provocation and seek other methods of dispute resolution rather than resorting to violence.
According to the Chief Medical Director of the hospital, Professor Adetokunbo Fabamwo, with the level of innovative solutions that LASUTH is bringing to Lagosians through its dedicated healthcare workers, it can only be done in an atmosphere free of chaos and agitation.
Violence against healthcare workers is unacceptable. It harms the psychological and physical well-being of the staff but also affects their job motivation.
“The management of the hospital, under any circumstances, would not tolerate any assault against her staff going forward. The hospital provides for checks and balances within the hospital which is available to treat situations if they occur, and the hospital on several occasions appealed to aggrieved members of the public to seek redress through various channels.
“The hospital is committed to providing quality healthcare services to our patients and their relatives and we urge everyone to cooperate with our staff to facilitate their care,” he added.
As a responsible workplace, LASUTH has continued to investigate workplace violence incidents, risks, or hazards; provide training and education to employees who may be exposed to workplace violence hazards and risks; meet record-keeping requirements; and prohibit acts of discrimination or retaliation against employees for reporting workplace violence incidents, threats, or concerns.
It has become expedient, therefore, for policymakers, hospital managers, and supervisors should work collaboratively to minimize workplace violence and ensure the safety and psychophysical stability of all healthcare workers in Lagos and the nation at large.
Olutayo Irantiola is an astute PR Consultant and Public Affairs Analyst. He can be reached via [email protected] and he blogs on www.peodavies.com
Health
SpecSMART Eye Clinic Takes Affordable, Quality Care to Ikeja, Environs

By Modupe Gbadeyanka
The dream of residents of Ikeja and its environs enjoying affordable and quality care has now become a reality as a result of the opening of a new branch of SpecSMART Eye Clinic in the Opebi area of the capital of Lagos State.
SpecSMART Eye Clinic, a leading provider of optometry services in Lagos, commenced operations in Nigeria’s commercial capital in 2022.
Since then, it has been offering top-notch eye care to residents of the metropolis, especially those living on the Island. It has built a strong reputation for delivering high-quality primary eye care and optical products.
However, to extend its services to Lagosians living on the Mainland, it has now opened a new branch in Ikeja, reinforcing its commitment to providing accessible, affordable eye care to a wider community.
Business Post gathered that the clinic’s state-of-the-art services are supported by a team of skilled optometrists and opticians, utilizing cutting-edge digital equipment.
The new Ikeja location will offer a wide range of services, including Automated Eye Examinations using advanced digital equipment for precise diagnosis and personalized care.
In addition, clients will enjoy on-the-spot lens glazing for single vision, bifocals, and varifocals, with additional lens coatings, with services to be rendered seven days a week from 9 am to 9 pm on Mondays to Saturdays, and on Sundays and public holidays from 10 am 7 pm.
Also, the clinic has over 950 frames, ranging from affordable home brands to premium designer options, priced from N18,000, and has flexible appointment scheduling with 24-hour online booking via SpecSMART’s website.
The facility has partnerships with leading HMO providers in the country and offers glaucoma management and other essential eye health services.
According to the company, its introductory packages start from N30,000 and include consultation, frame, and single-vision lenses.
“With the opening of our Ikeja branch, we are ready to serve more individuals who need accessible, cost-effective, and reliable eye care.
“Our aim is to create a positive impact in Nigeria’s optometry sector by combining advanced technology with a patient-centred approach,” the Practice Head and Medical Director of SpecSMART, Dr Adaeze Nwoko, stated.

Health
FG Begins Vaccination Against Mpox in FCT, Six States

By Adedapo Adesanya
The Federal Ministry of Health and Social Welfare through the National Primary Health Care Development Agency (NPHCDA) has commenced the vaccination against Monkeypox, now known as Mpox.
Business Post reports that Bayelsa, Rivers, Cross River, Akwa Ibom, Enugu, Benue, and the Federal Capital Territory, were selected as pilot states for the vaccination.
An average of 631 persons are expected to be vaccinated across the seven states with two doses of the Mpox vaccine. A buffer for 50 persons will be kept at the national in case of an upsurge in other states.
NPHCDA in a statement posted on its verified X account confirmed the exercise, stressing that the vaccination will help to protect communities and safeguarding health of the people.
In a related development, according to the latest update by the Nigeria Centre for Disease Control (NCDC), there are 1,442 suspected cases of Mpox from 36 states and the Federal Capital Territory, while the number of confirmed cases of the infection was 118 from 28 states and the FCT.
“To prevent the spread of Mpox, we strongly advise the public to avoid contact with animals that may carry the virus, including sick or dead animals in affected areas, avoid handling materials that have been in contact with infected animals, limit unnecessary physical contact with individuals who are infected, practice frequent handwashing with soap and water, and ensure that animal food products are thoroughly cooked before eating.
“It’s also important to use protective clothing and gloves when handling sick animals or their tissues. Similarly, health workers are advised to follow standard safety protocols including droplet precautions when treating patients, use protective equipment including masks, gloves, and gowns, during patient care, and be vigilant for symptoms of Mpox, especially fever and rash, among other measures.”
Health
AXA Mansard Health Partners LUTH in Blood Donation Drive

By Aduragbemi Omiyale
Over 250 pints of blood have been donated by AXA Mansard Health to the Lagos University Teaching Hospital (LUTH), Idi Araba.
The blood was donated by more than 100 employees of the leading health insurance company in Nigeria through its volunteering programme tagged AXA Hearts in Action.
The initiative is part of the company’s blood donation drive aimed at contributing to positive societal and environmental impacts through employee volunteering, and expertise related financial support and in-kind donations.
According to the Chief Client Officer of AXA Mansard, Ms Rashidat Adebisi, “Through the AHIA, our employees do not just give time to great causes; we work together for a better future.”
“We share our time, knowledge and expertise as a people with a shared purpose of acting for human progress by protecting what matters through initiatives like this,” she added.
Ms Adebisi said the blood drive is a shining example of the philosophy in action, where collective contributions serve as a reminder that true impact often involves giving more than just money. It’s about putting one’s heart in action – an idea embedded in AXA’s corporate culture.
On his part, the chief executive of AXA Mansard Health Limited, Mr Tope Adeniyi, said with hospitals frequently experiencing blood shortages, events like these serve as a lifeline for patients in need.
“We are proud to contribute to the local healthcare sector and provide much-needed support to hospitals such as LUTH, ensuring that they have resources essential to saving lives,” he added.
Also commenting, the Head of Corporate Services and Public Relations at LUTH, Omolola Olubukunola Fakeye, thanked the firm for the “generous support,” which has made a “meaningful difference to our blood bank and ultimately to the lives of patients.”
“Blood donations are invaluable in many critical treatments, and initiatives like AXA Mansard’s blood drive bring immense relief to healthcare system.
“We are sincerely grateful for this partnership and the dedication of AXA Mansard’s employees,” Fakeye stated.
AXA Hearts in Action operates globally, she urging AXA employees everywhere to engage with and give back to their communities.
Through diverse projects – from health initiatives like this blood drive and medical outreaches to environmental efforts like the AXA Week for Good “Trash-to-Treasure” waste management project – AXA staff have opportunities to make a lasting difference on issues that matter.
For AXA Mansard, every act of social service brings them closer to the communities they serve, helping build a world where giving back is not only about charity but about lasting, positive change.
-

 Feature/OPED5 years ago
Feature/OPED5 years agoDavos was Different this year
-
Travel/Tourism8 years ago
Lagos Seals Western Lodge Hotel In Ikorodu
-

 Showbiz2 years ago
Showbiz2 years agoEstranged Lover Releases Videos of Empress Njamah Bathing
-

 Banking6 years ago
Banking6 years agoSort Codes of GTBank Branches in Nigeria
-

 Economy2 years ago
Economy2 years agoSubsidy Removal: CNG at N130 Per Litre Cheaper Than Petrol—IPMAN
-

 Banking2 years ago
Banking2 years agoFirst Bank Announces Planned Downtime
-

 Sports2 years ago
Sports2 years agoHighest Paid Nigerian Footballer – How Much Do Nigerian Footballers Earn
-

 Technology4 years ago
Technology4 years agoHow To Link Your MTN, Airtel, Glo, 9mobile Lines to NIN























